Last updated April 2025
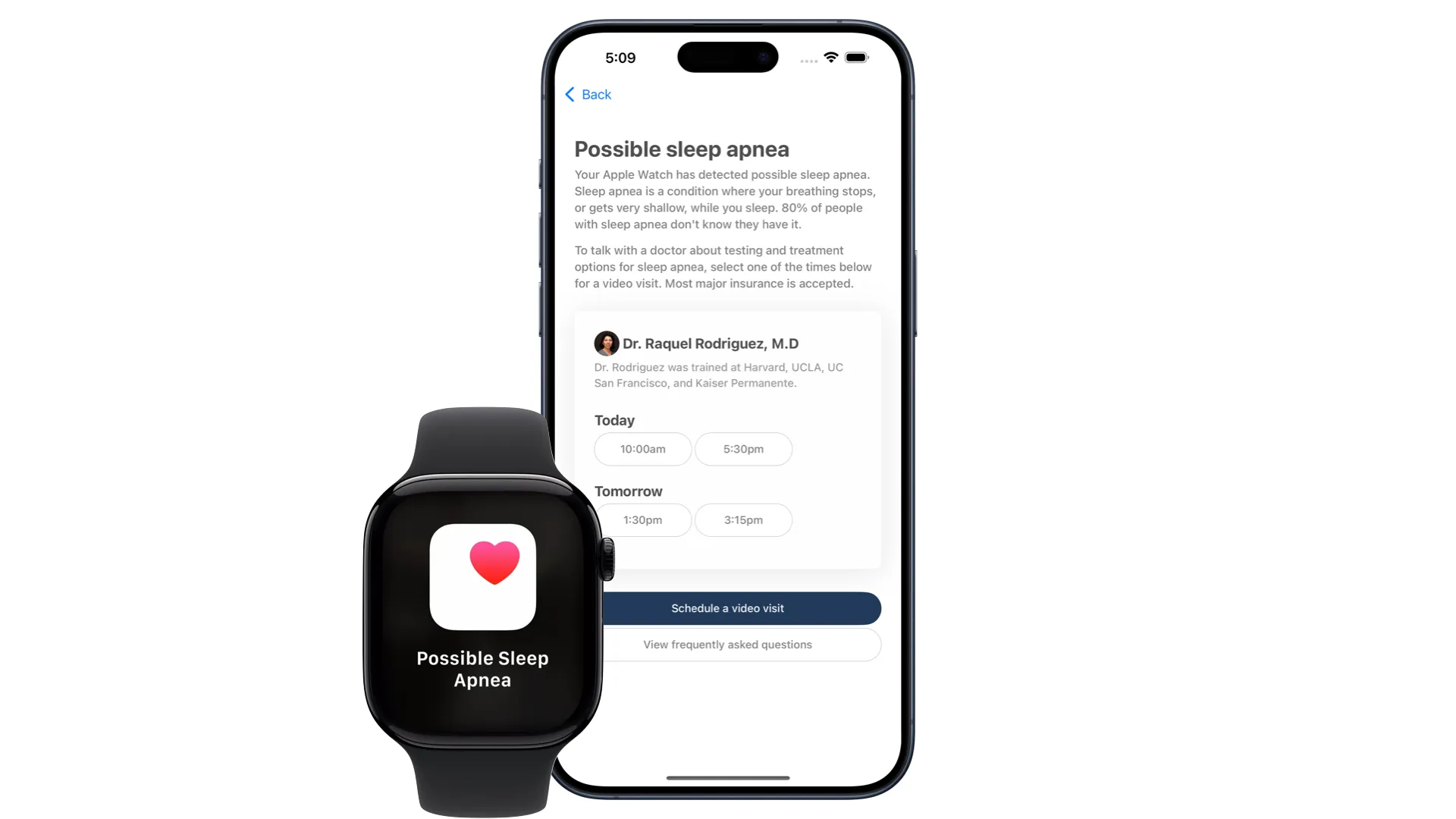
Apple Watch can now detect possible sleep apnea. This feature, called breathing disturbances, was cleared by the FDA in September 2024 and is now widely available on the Apple Watch Series 9, Series 10, and Ultra 2.
In 2017, I helped run the first research study that detected sleep apnea using Apple Watch and a deep neural network. In this post, I’ll explain the accuracy of Apple Watch’s sleep apnea algorithm, the science on-the-wrist sleep apnea detection (including techniques like peripheral arterial tone), what to do about sleep apnea alerts, and the potential impact of widespread sleep apnea screening (80% of sleep apnea is undiagnosed).
Accuracy: Apple Watch detects 89% of severe sleep apnea
Apple Watch is 89% accurate at detecting severe sleep apnea. It detects 43% of moderate cases. In technical terms, the Apple Watch’s sensitivity for severe sleep apnea is 89%, and its specificity is 98.5%.
What does this mean? If you get a sleep apnea alert, you shoudl take it seriously. If you don’t get a sleep apnea alert, it’s still possible you have moderate sleep apnea.
The FDA cleared the Apple Watch to detect—but not diagnose—possible sleep apnea. To get diagnosed, you need to complete an at-home sleep apnea test ordered by a doctor. Empirical Health doctors can help with sleep apnea testing and treatment.
 An at-home sleep apnea test. Empirical Health doctors treats sleep apnea in 30+ US states.
An at-home sleep apnea test. Empirical Health doctors treats sleep apnea in 30+ US states.
The science behind Apple Watch sleep apnea detection
Obstructive sleep apnea is a condition when you stop breathing during sleep, causing your blood oxygen levels to fall. The more often this happens, the more severe the sleep apnea. This frequency of nighttime apnea events is called the Apnea-Hypopnea Index (AHI).
Previous sleep apnea tests measured five channels: pulse (heart rate), blood oxygen saturation, snoring, nasal flow, and chest motion. On the wrist, only the first three channels are available.
Sleep apnea signals measurable from wrist-based sensors
Two “tricks” help us infer the presence of apnea events without nasal flow or chest motion:
- Peripheral arterial tone. In 2019, the FDA approved the first sleep apnea test, the WatchPAT 1, to use a new technique called peripheral arterial tone. Unlike traditional sleep apnea tests, peripheral arterial tone can be measured entirely with sensors on the wrist. We’ll go deeper on peripheral arterial tone in the next section.
- Cardiovascular signals. Our 2017 study used only heart rate and step count as raw inputs into a deep neural network (an LSTM, at the time). Nowadays, the Apple Watch calculates 20+ metrics of health across multiple organ systems, including several heart health metrics. I just performed an updated analysis that showed 5 of the top 10 predictors of sleep apnea risk are cardiovascular in nature. These heart signals, even if of modest individual accuracy, may help accurately detect sleep apnea when combined.
Apple Watch’s sleep apnea algorithm currently uses only 3D accelerometer data
Surprisingly enough, Apple Watch’s algorithm doesn’t use blood oxygen saturation. It only uses 3D accelerometer data, according to Apple’s own report. This is likely so that sleep apnea detection can work without being subject to the current patent dispute which has disabled the Apple Watch’s oxygen sensor.
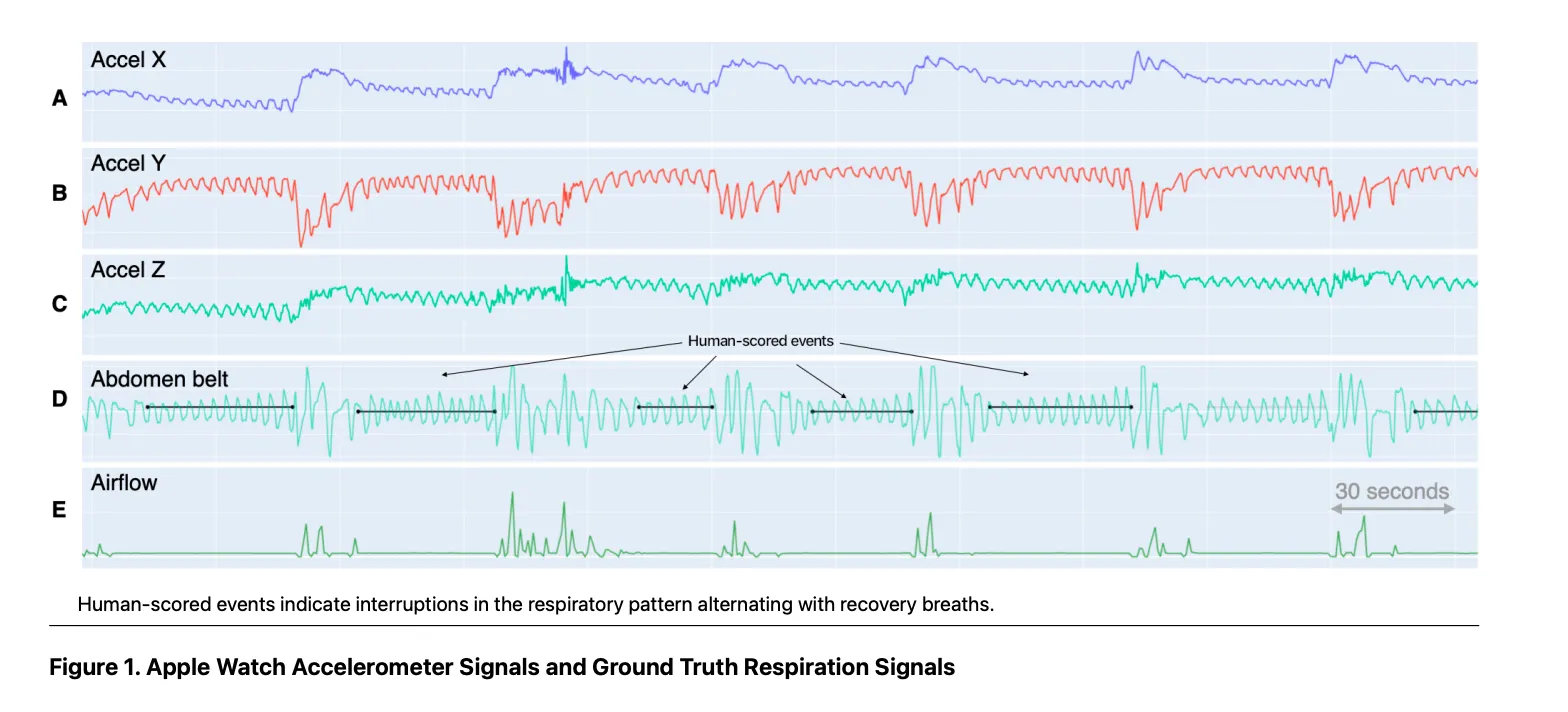
So why would accelerometer data be enough to detect likely sleep apnea? The intuition relates to something called peripheral arterial tone.
Peripheral arterial tone, sleep apnea, & the autonomic nervous system
Peripheral arterial tone (PAT) measures variations in arterial volume, which reflects the activity of the autonomic nervous system (ANS).
The ANS controls involuntary bodily functions, including heart rate. You can think of the ANS as a constant “tug of war” between two halves: the sympathetic nervous system (“fight or flight”) and the parasympathetic nervous system (“rest and digest”). When the sympathetic nervous system dominates, heart rate is higher, heart rate variability is low, and your arteries tensen. When the parasympathetic system dominates, heart rate is lower, HRV is high, and your arteries are less tense.
During episodes of apnea (when breathing stops during sleep), the body’s oxygen levels drop, triggering a surge in sympathetic activity to compensate. This response can cause significant fluctuations in PAT, which allows a wrist-based device to pick up on the apnea event.
WatchPAT ONE: the first wrist-based sleep apnea diagnostic
In 2019, the FDA cleared the first medical device to use peripheral arterial tone to test for sleep apnea — the WatchPAT ONE. This cleared the way for manufacturers of consumer wearables, like Apple and Samsung, to build algorithms that detect sleep apnea.
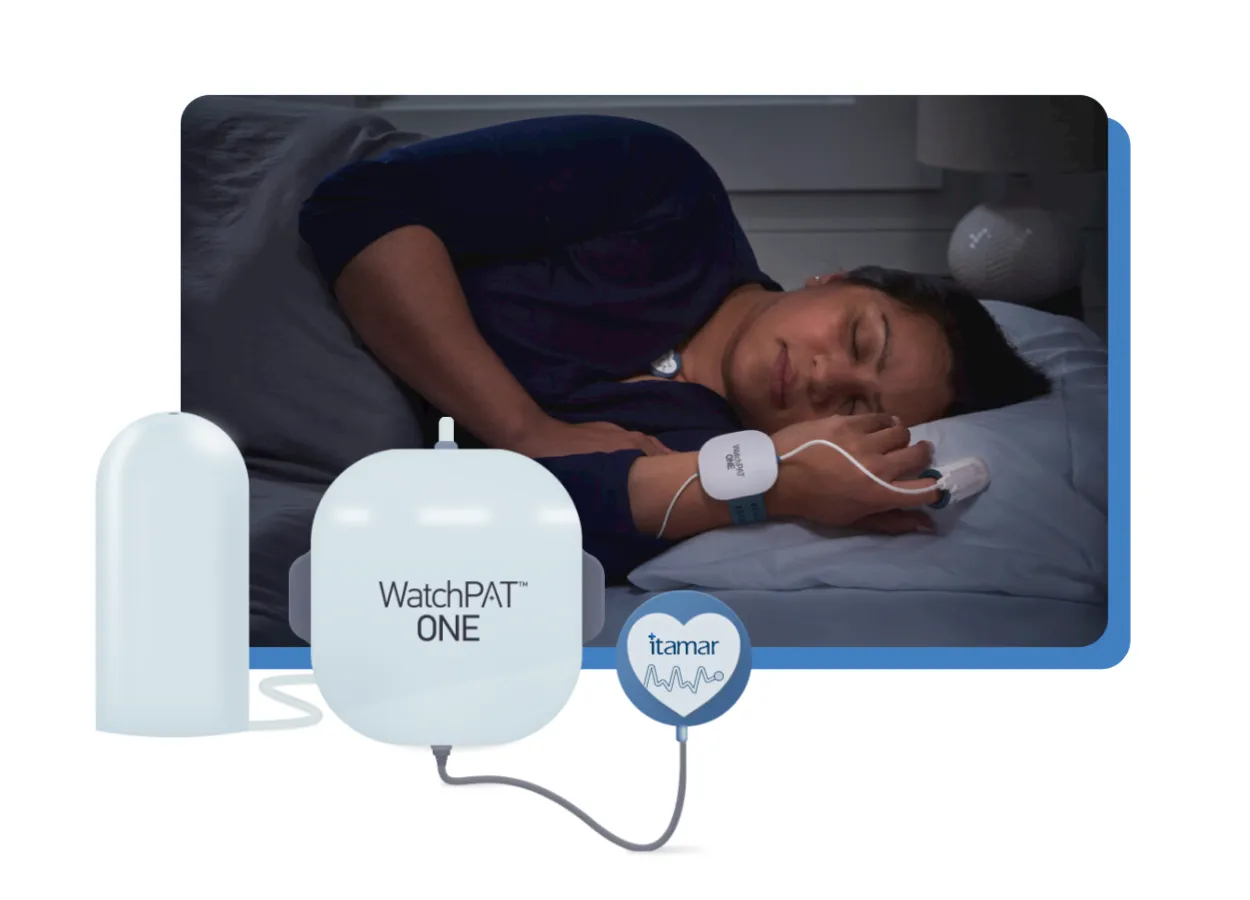
If Apple Watch detects possible sleep apnea, you’ll need to confirm it using an at-home test like the WatchPAT ONE.
Apnea-hypopnea-index (AHI) vs Apple Watch breathing disturbances
Ultimately, the output of all sleep apnea diagnostics is a number: the apnea-hypopnea-index (AHI). The AHI is the number of apnea or hypopnea events per hour. Low severity sleep apnea is 5-14, medium severity sleep apnea is an AHI of 15-29, and high severity sleep apnea is an AHI of 30 or more.
Is peripheral arterial tone accurate for detecting sleep apnea? In a word, yes. A 2013 meta-study showed high correlation (0.89) between PAT and conventional sleep testing. Subsequent studies have validated the technology in patients with COPD and atrial fibrillation. Future features around blood pressure detection on Apple Watch would be based on similar science.
Apple Watch’s breathing disturbance metric roughly correlated with AHI. However, since the watch is designed for high specificity (low false positives), you can’t use breathing disturbances as a proxy of AHI if you have diagnosed sleep apnea.
What’s the impact of Apple Watch sleep apnea screening?
80% of sleep apnea cases are undiagnosed. Undiagnosed sleep apnea affects more than 23.5 million people in the US alone. The complications of untreated sleep apnea—such as car crashes or heart attacks—cause $150B of wasted spend every year.
What to do if Apple Watch says possible sleep apnea
If your Apple Watch says you have possible sleep apnea, a doctor needs to prescribe a sleep test. Most insurance covers
at-home sleep testing. In some cases, it may be medically necessary to do an overnight sleep study in a lab.
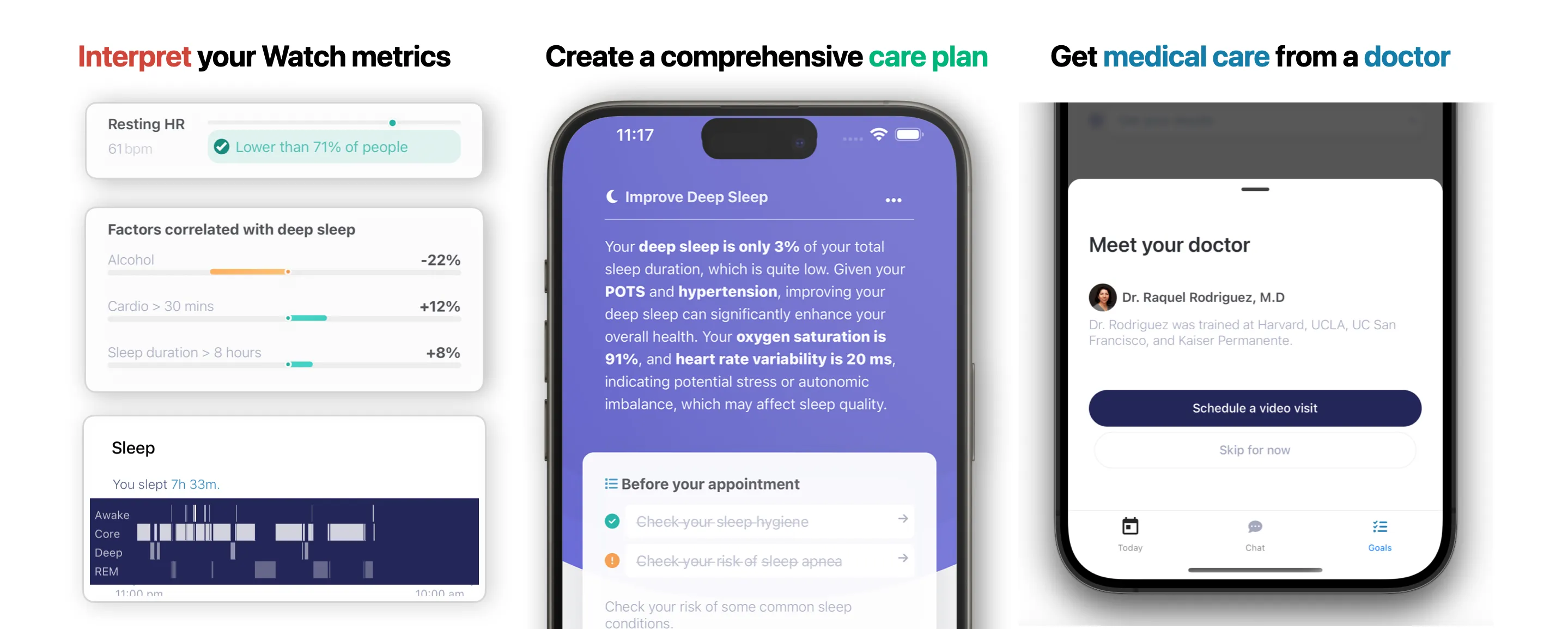
Doctors at Empirical Health can help you get tested for sleep apnea. We usually prescribe an at-home sleep test, unless an in-lab test is medically necessary, and we typically work with you to find tests covered by your health insurance. Your Empirical Health doctor appointment is covered by most insurance.






