Chronic inflammation has long been known to double your risk of heart disease, but prior to now, inflammation has never been a SMuRF: standard modifiable risk factor for heart disease.
The American College of Cardiology just released recommendations that change that. The ACC is now recommending that everyone measure inflammation (hs-CRP) via a blood test:
Because clinicians will not treat what they do not measure, universal screening of hsCRP in both primary and secondary prevention patients, in combination with cholesterol, represents a major clinical opportunity and is therefore recommended. American College of Cardiology
“hs-CRP” stands for high-sensitivity c-reactive protein. A standard c-reactive protein (CRP) test measures levels above 10 mg/L (common in infections), whereas hs-CRP measures lower levels of chronic inflammation (an indicator of heart disease). CRP is an inflammatory marker produced by the liver in response to tissue damage or infection.
There were many interesting pieces of evidence that led to the recommendation to screen using hs-CRP. The whole article, published in JACC, is worth a read, but this blog post extracts a few of the most interesting parts — or at least, the parts I thought were most interesting.
Inflammation (hs-CRP) is a stronger predictor of heart disease than cholesterol
For decades, LDL cholesterol (or ApoB) has been the main focus of cardiovascular risk assessment. But this chart shows hs-CRP is actually a stronger predictor of cardiovascular events than LDL.
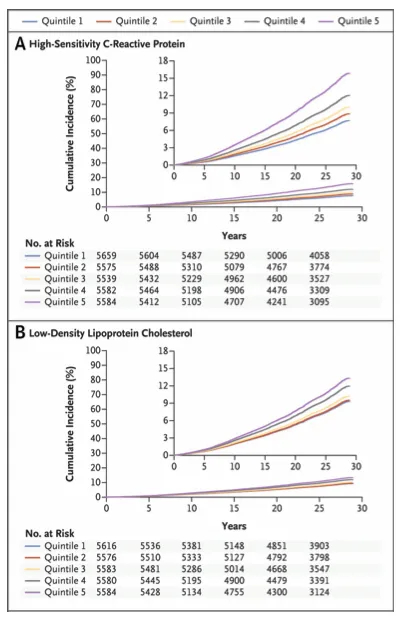
Why? In some ways, cholesterol has become a victim of its own success. We now screen the whole population for high cholesterol, give statins to those with high LDL (or ApoB), and so then the majority of people who end up having heart attacks have lower cholesterol than they would naturally have. This means most of the majority of residual risk for heart attacks will be found in biomarkers that aren’t SMuRFs.
Inflammation (hs-CRP) is one such non-SMuRF, perhaps one of the strongest. This is especially true for people already on statins or those without traditional risk factors (sometimes called “SMuRF-less” patients). In these groups, cholesterol may be well controlled, but inflammation remains a key driver of events.
Of course, other traditional risk factors matter in addition to inflammation. Everyone shoudl still measure blood pressure, HbA1c or insulin resistance, eGFR (kidney function), LDL cholesterol or ApoB, Lp(a), and so on.
Ways to lower inflammation
The ACC consensus reviewed a range of clinical trials. They included both drugs and lifestyle interventions for lowering inflammation and reducing cardiovascular risk. If your hs-CRP is high, these are the best evidence-based ways to reduce it:
| Trial Name | Drug (Class) | Sample Size (n) | Population/NYHA Functional Class | Follow-Up | Primary Endpoint | Treatment Outcome |
|---|---|---|---|---|---|---|
| ATTACH | Infliximab (TNF inhibitor) | 150 | NYHA III/IV HF | 7 mo | Clinical status (composite score) | No improvement or worsening; deaths highest in high-dose infliximab |
| ACCLAIM | IVIG | 2314 | NYHA II-IV HF | 10.2 mo | Composite all-cause mortality and CV hospitalization | No reduction in events; trend toward benefit in NYHA III and IV |
| CANTOS | Canakinumab (anti–IL-1β) | 10,061 | Prior MI; hsCRP ≥2 mg/L | 3.7 y (median) | Nonfatal MI, nonfatal stroke, or CV death (MACE); HF-related mortality | Reduced MACE and HF events; no effect on all-cause mortality; primary endpoint events: 3.86% vs 4.50% |
| CIRT | Methotrexate | 4,786 | Stable MI plus CAD | 2.3 y (median) | CV event rates | No effect on CV events, inflammation, or lipids |
| CLEAR SYNERGY | Colchicine | 3,056 | Acute MI plus PCI | 22.6 mo | Death from CV causes, recurrent MI, ischemic stroke | No significant difference in primary endpoint |
| COLCOT | Colchicine | 4,745 | Acute MI patients | 22.6 mo | CV event rates | CV events lower than placebo |
| LoDoCo2 | Colchicine | 5,522 | Stable CAD | 28.6 mo | Composite of CV death, nonfatal MI, ischemic stroke, or ischemia-driven revasc. | CV events lower than placebo |
| GISSI-HF | Rosuvastatin (statin) | 4,574 | NYHA II-IV HF | 3.9 y | All-cause mortality and CV hospitalization | No effect on primary endpoints |
| JUPITER | Rosuvastatin (statin) | 17,802 | No CVD / LDL <130 mg/dL; hsCRP ≥2 mg/L | 1.9 y (median) | MI, stroke, arterial revascularization, hospitalization for unstable angina, or CV death | Reduced events (HR 0.56–0.69) |
| CORONA | Rosuvastatin (statin) | 5,011 | NYHA II-IV HF; ischemic etiology | 32.8 mo | CV death, nonfatal MI, nonfatal stroke | No effect on primary endpoint |
| OPT-CHF | Etanercept (TNF inhibitor) | 1,500 | NYHA II-IV HF | 6 mo | Death, hospitalization, or worsening HF | No effect on primary endpoint |
| DCMP | Prednisone (corticosteroid) | 84 | NYHA II-IV HF; biopsy-proven myocarditis | 5.7 and 12.3 mo | Improvement in LVEF, survival, or combined outcome of death or transplantation | No significant benefit |
| RENEWAL | Etanercept (TNF inhibitor) | 2,048 | NYHA II-IV HF | 6 mo | Composite outcome of death or hospitalization | No effect on primary endpoint |
If your hs-CRP is high, here’s what works to lower inflammation:
- Statins lower both hs-CRP and LDL. Clinical trials show a substantial reduction in cardiovascular events, even when LDL is normal (JUPITER trial).
- Colchicine: Reduces recurrent events in people with established heart disease (COLCOT, LoDoCo2).
- Lifestyle: Anti-inflammatory diets (Mediterranean, DASH), regular exercise, smoking cessation, and maintaining a healthy weight all lower hs-CRP and reduce cardiovascular risk.
What doesn’t work? Some anti-inflammatory drugs (methotrexate, TNF inhibitors, corticosteroids) have not shown benefit in major trials.
What’s a normal range for hs-CRP? What’s a high hs-CRP?
A good hs-CRP is below <1 mg/L. hs-CRP above 3 mg/L is high risk.
This chart shows risk of cardiovascular events (y axis) vs various levels of hs-CRP:
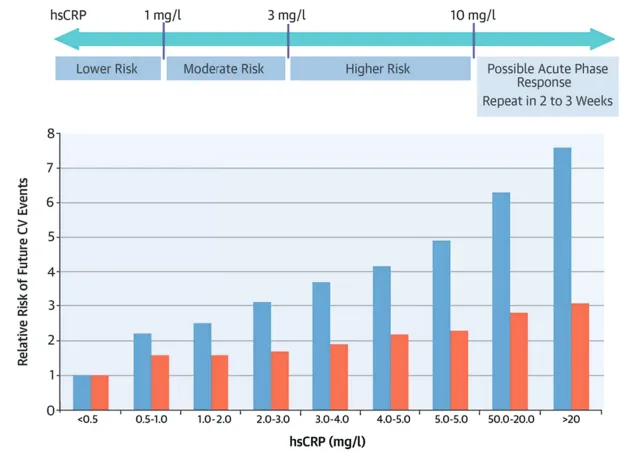 hs-CRP vs risk of heart disease. Blue bars represent relative risk; orange bars represent risk after adjustment for traditional risk factors like LDL and blood pressure. Source: JACC
hs-CRP vs risk of heart disease. Blue bars represent relative risk; orange bars represent risk after adjustment for traditional risk factors like LDL and blood pressure. Source: JACC
Interpreting your individual situation with a doctor is important, since medications may change your hs-CRP. For example, statins tend to lower hs-CRP levels for both women and men. Women on hormone replacement therapy sometimes have elevated hs-CRP levels.
What’s the best biomarker of inflammation? hs-CRP vs other blood tests.
According to the American College of Cardiology, hs-CRP is the best biomarker of inflammation. The ACC evaluated several other markers: IL-6, fibrinogen, neutrophil-to-lymphocyte ratio, EPA/AA ratio, and serum amyloid A. While these markers have also been shown to predict cardiovascular risk, once hs-CRP is known, the others don’t add more signal.
In other words, you’re best off simply measuring hs-CRP with a blood test, and then spending money elsewhere on heart health.
Other insights on inflammation and heart health
The JACC article is packed with other interesting insights. These ones stood out to me:
- Imaging biomarkers (like CT, PET, MRI, and perivascular “fat attenuation index”) can detect vascular inflammation and may help predict coronary events, but are not yet ready for routine clinical use.
- Bempedoic acid is a newer cholesterol-lowering drug that also lowers hs-CRP, but its long-term outcomes are still being studied.
- Colchicine (0.5 mg/d) is now FDA-approved as an adjunct for secondary prevention in stable ASCVD, but should be avoided in people with significant kidney or liver disease.
- Novel IL-6 inhibitors are being studied as future anti-inflammatory therapies for heart disease.
What’s the cost of an hs-CRP blood test?
You can buy a comprehensive blood test with hs-CRP for under $200. Empirical Health’s comprehensive health panel is one option. For the most part, hs-CRP is not currently covered by health insurance.
How to get a lab test for hs-CRP and cholesterol
Blood tests for hs-CRP are widely available and inexpensive. Empirical Health’s comprehensive health panel is one option. Since the ACC now recommends both routine hs-CRP testing for both people at risk (primary prevention) and those with established heart disease (secondary prevention).
Get your free 30-day heart health guide
Evidence-based steps to optimize your heart health.
