Elevated Lipoprotein(a) is the single strongest inherited risk factor for heart disease.
While cholesterol tests are standard, different types of cholesterol particles vary in how strongly they cause heart disease. Lipoprotein(a) measures a type of cholesteorl particle that’s 6x more atherogenic than standard LDL cholesterol.
Lp(a) is mostly inhereted. Levels vary 100-fold between people, and 80–90% of that variation is genetic (stable by age 5). Leading experts—Peter Attia and Sotirios Tsimikas—rank Lp(a) alongside ApoB as a must-test biomarker whose heritability surpasses hypertension, diabetes, or obesity. The American College of Cardiology recommends measuring Lp(a) at least once.
What counts as a “normal” Lp(a) level? How much does elevated Lp(a) boost your risk of cardiovascular disease? What does a blood test cost? Are there proven ways to lower Lp(a)? Read on for answers.
What is Lp(a)? How is it different than LDL?
An Lp(a) particle is just an LDL particle wrapped with an extra protein, apoprotein (a) [1]. The extra protein camoflauges the particle from the receptors in your liver [2].
Each LDL particle itself contains one ApoB protein, 1,500 cholesterol molecules on average, and about 6% triglycerides. For most people, about 4-13% of LDL particles will be an Lp(a) particle. In other words, for each LDL particle with the wrapper protein, there will be 8-25 LDL particles without it. [3]
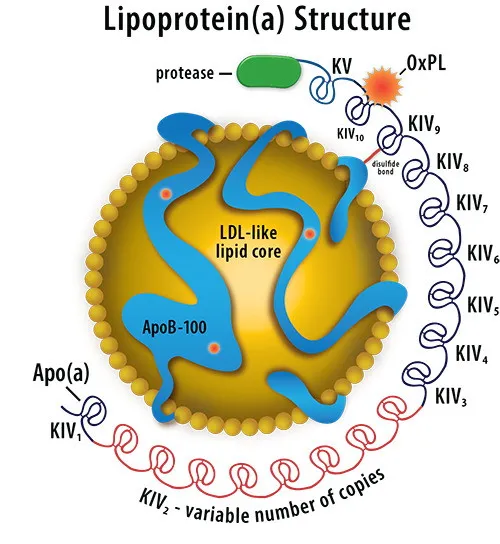 Lipoprotein(a) particle = an LDL core, an ApoB structural protein, and an apoprotein (a) protein wrapping the whole structure.
Lipoprotein(a) particle = an LDL core, an ApoB structural protein, and an apoprotein (a) protein wrapping the whole structure.
One study estimates that each Lp(a) particle is 6.6x more atherogenic than each “ordinary” LDL/ApoB particle. The study itself used a Mendelian randomization analysis, and found a 50 nmol/L increase in genetically-determined Lp(a) corresponded to a 28% higher odds of cardiovascular disease. (In contrast, LDL-associated ApoB led to only a 4% increase).
The reasons why Lp(a) is more atherogenic is an active area of research, but is believed to be because Lp(a) promotes inflammation, increases clotting, and inhibits clearance by the liver.
Elevated Lp(a) and cardiovascular disease
How does high Lp(a) affect your risk of heart disease? If your Lp(a) is above 100 mg/dL, your overall risk of cardiovascular disease is 114% higher. The following chart on Lp(a) levels shows how your risk of a cardiovascular event (MACE: major adverse cardiac event) changes from the bottom quartile of Lp(a) to the top quartile.
Lipoprotein(a) levels chart
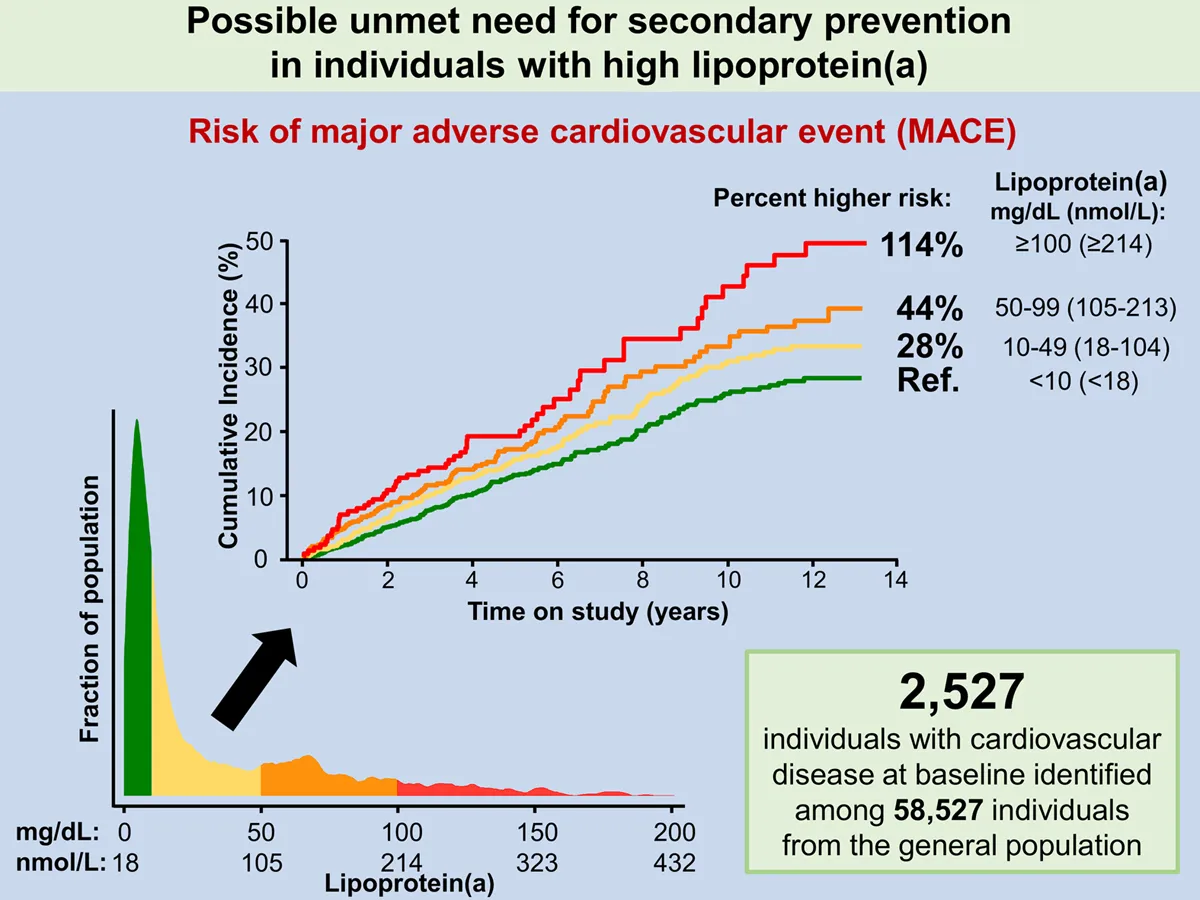 Chart of Lipoprotein(a) levels vs risk of cardiovascular events. Source: European Heart Journal
Chart of Lipoprotein(a) levels vs risk of cardiovascular events. Source: European Heart Journal
The above chart shows that people with an Lp(a) of 10-49 mg/dL have 28% higher cardiovascular risk. People with an Lp(a) of 50-99 mg/dL have 44% higher cardiovascular risk. And those in the top quartile, >100 mg/dL, have 114% higher risk of cardiovascular disease.
Life expectancy with high lipoprotein(a)
In a study of 18,720 participants, being at the 95th percentile of Lp(a) levels was equivalent to being 1.5 years older in chronological age. So your life expectancy with high Lp(a) is about 1.5 years shorter.
Normal range for the Lipoprotein(a) blood test
A normal Lp(a) is 30 mg/dL or less. Optimal Lp(a) is 14 mg/dL or less. Elevated Lp(a) is 50 mg/dL or above. Lp(a) concentrations can vary from <1 to >200 mg/dL, with 25% of people reaching 150 mg/dL or more.
Normal vs elevated Lp(a) range in nmol
Most labs report Lp(a) as mg/dL (mass), not particle count (nmol/L). Furthermore, the guidelines from the American College of Cardiology, Canadian Cardiovascular Society, European Atherosclerotic Society, and National Lipid Association use slightly different thresholds.
But in general:
- above 125 nmol/L is always considered high Lp(a)
- Below 75 nmol/L is normal Lp(a)
- Between 75-125 nmol/L is considered intermediate or elevated Lp(a), with specific numbers depending on the guideline used.
How much does an Lp(a) blood test cost?
An Lp(a) test costs about $50 on its own. Most people will measure Lp(a) as part of a comprehensive heart health panel including ApoB ($50), hs-CRP ($65), a lipid panel ($40), and likely other biomarkers like A1c (blood sugar), cell counts, and more.
 Empirical Health’s comprehensive heart health panel costs $190,
includes Lp(a), ApoB, hs-CRP, 90+ other biomarkers, and a comprehensive care plan from an MD.
Empirical Health’s comprehensive heart health panel costs $190,
includes Lp(a), ApoB, hs-CRP, 90+ other biomarkers, and a comprehensive care plan from an MD.
How to lower Lp(a)
While statins are popular drugs to lower LDL cholesterol or ApoB, there are no drugs FDA-approved for the indication of lowering Lp(a). However, there are nutritional approaches with moderate evidence, as well as medications in the research phase.
Using Niacin (Vitamin B3) to naturally lower Lp(a)
Niacin reduces Lp(a) by 15% to 25%. Each 10 mg/day increment in dietary niacin is associated with a 9% lower odds of ASCVD.
Nutritional yeast has the highest amount of niacin per serving, with 1 tbsp containing the daily requirement. (Marmite, a British spread, is made from yeast.) Other foods high in niacin are liver, chicken breast, tuna, turkey, salmon, anchovies, pork, Peanuts, Avocado, Brown Rice, peas, and many fortified foods (e.g. cereals).
However, there’s a caveat. A clinical trial of niacin supplements showed no reduction in cardiovascular events. So is niacin a cause of lower cardiovascular events, or a marker of a good diet? This situation is similar to HDL. Some evidence from prospective cohorts shows benefits of dietary niacin, as opposed to supplements. On the balance, you’re best of focusing on major nutrients first (fiber, sodium, potassium, saturated fat, etc), getting those right, then adding in secondary nutrients like niacin.
How to lower lipoprotein(a) with medication
Two medications for Lp(a) are on the horizon: PCSK9 inhibitors (FDA-cleared, but expensive) and lepodisiran (an si-RNA therapy).
PCSK9 inhibitors lower Lp(a), but are expensive
PCSK9 inhibitors are FDA-approved to lower LDL cholesterol (or ApoB). Since they operate on a different pathway than statins, they’re usually prescribed alongside a statin for a “double” benefit. As an added bonus, PCSK9 inhibitors reduce Lp(a) by 20-30%.
However, PCKS9 inhibitors are expensive. The list price of Praluent is $5,850 per year, and insurance coverage is currently very limited. For example, United Healthcare’s coverage policy specifies that patients need to meet all of six criteria, including already being on statins at the maximum dose, in order to qualify for coverage of PCKS9 inhibitors.
A new drug, lepodisiran, lowered Lp(a) by 93.9% in a clinical trial
In a Phase II clinical trial, a new si-RNA therapy (lepodisiran) lowered Lp(a) by 93.9%. These results were presented at the American College of Cardiology 2025 Scientific Sessions. A Phase 3 clinical trial is estimated to complete in 2029, and if things go well, FDA approval and eventually insurance coverage will follow that. The Lp(a)HORIZON trial is testing a second drug, Pelacarsen, which is also an si-RNA therapy. Data from Lp(a)HORIZON is expected in the first half of 2026.
If you can’t directly lower Lp(a), what can you do?
Since drugs that directly lower Lp(a) are either expensive or not expected until after 2029, what can you do about high Lp(a)? Most experts recommend aggressively managing ApoB—using nutrition, medication, and exercise to bring your ApoB down to a lower level than you would otherwise choose.
The bottom line: how and why test your Lp(a)
If you want to get your Lp(a) tested, Empirical’s comprehensive heart health panel includes Lp(a), ApoB, hs-CRP (inflammation), cholesterol, and more, as well as dedicated care plans that help you choose nutrition, medication, and exercise.
Footnotes
[1] Apoproteins are a class of proteins, of which apolipoproteins (such as ApoB) are a subset. Apoprotein (a) is a glycosylated protein (i.e., it has sugar molecules attached), which consists of a repeated protein domain, kringle IV. The number of repetitions is determined by our genes and correlated with cardiovascular risk.
[3] Technically the apoprotein (a) camouflages the LDL particle from your hepatic receptors, which exist mostly in the liver but also exist in your intestine, kidney, brain, and adipose tissue.
[3] This calculation is based on Particle Number and Characteristics of Lipoprotein(a), LDL, and apoB: Perspectives on Contributions to ASCVD, which is itself a response to this study based on the UK Biobank data.
“For example, Lp(a) levels are typically <75 nmol/L (<30 mg/dL) and highly elevated levels are approximately 250 nmol/L (approximately 100 mg/dL). In contrast, untreated apoB levels are approximately 100 mg/dL or 1,949 nmol/L (to convert apoB in mg/dL to nmol/L, multiply by 19.49 using a molecular weight of apoB-100 of 513,000 daltons that does not include glycosylation modifications), and LDL-C 130 mg/dL or 3.36 mmol/L (to convert LDL-C in mg/dL to mmol/L divide by 38.67), or 2,360,000 to 3,320,000 nmol/L. Thus, even though individual Lp(a) particles may be more atherogenic at the per-particle level, the sheer relative excess of apoB and cholesterol molecules on LDL particles contributes globally to a higher risk at the individual level and for population-based risk.”
Get your free 30-day heart health guide
Evidence-based steps to optimize your heart health.
