It’s almost a cliche: a middle-aged dad who feels generally fine, skips annual checkups, ignores that persistent chest tightness, and dismisses his family’s reminders to see the doctor, until one day he shows up in the ER with crushing chest pain and is diagnosed with a heart attack.
A new study followed a cohort of 5,112 people for 35 years (from 1985 to 2020). it found men reach a 5% cumulative incidence of cardiovascular disease (CVD) about 7 years earlier than women. The gap begins in your 30’s and then widens, and traditional cardiovascular risk factors don’t fully explain the gap.
In the rest of this post, we’ll go into what the study found, risk factors you can assess, and how these results might change medical practice.
The gap is almost entirely coronary heart disease
The study tracked four subtypes of cardiovascular disease: coronary heart disease (CHD), stroke, heart failure, and CVD overall.
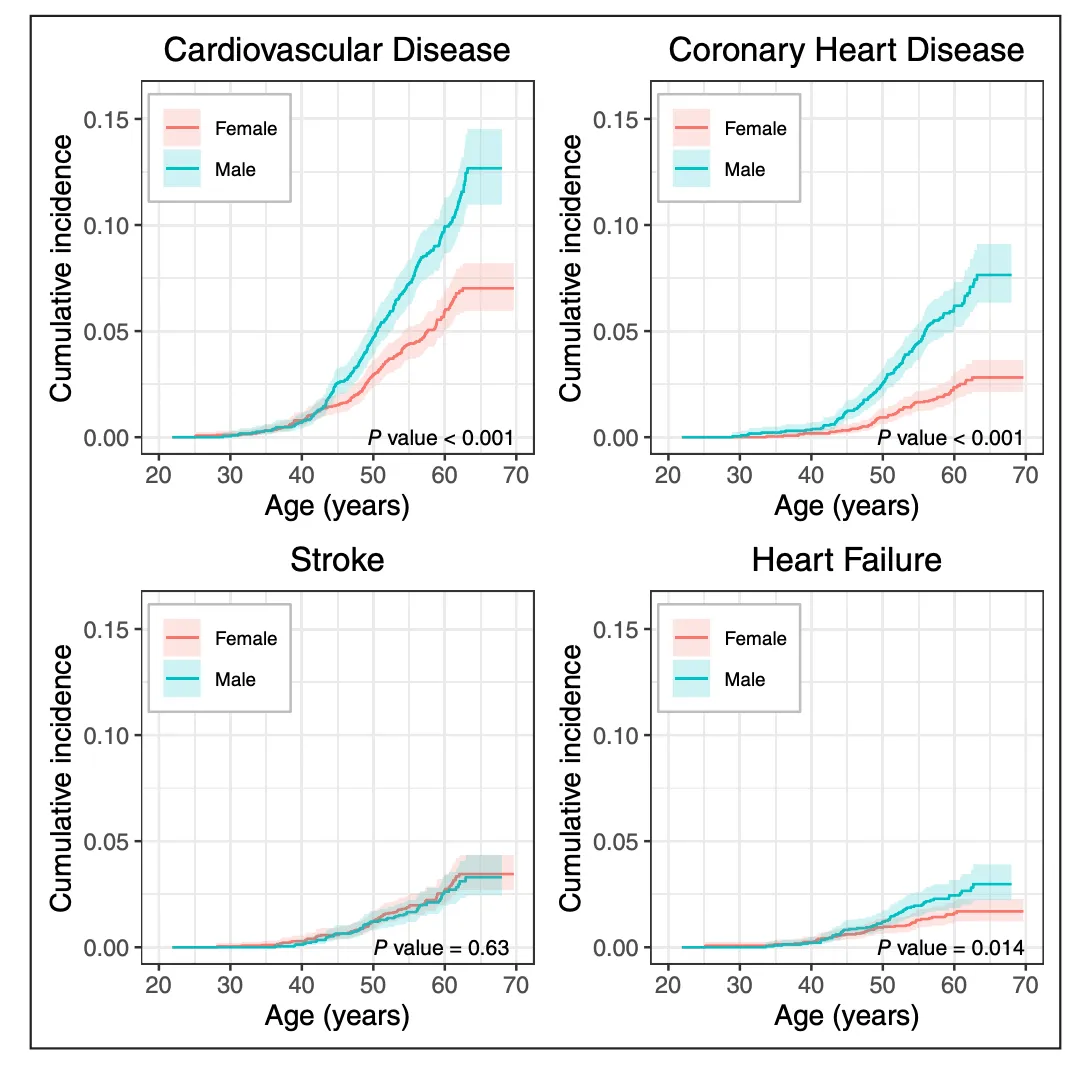 Cumulative incidence of cardiovascular disease in men (blue) and women (red) across four subtypes.
Cumulative incidence of cardiovascular disease in men (blue) and women (red) across four subtypes.
Coronary heart disease is where the gap is widest. Men reached a 2% cumulative incidence of CHD roughly 10 years before women. This confirms what cardiologists have long observed: the CHD age gap hasn’t narrowed despite decades of public health progress. Stroke shows essentially no sex difference in early and mid-adulthood. Men and women had nearly identical ages of onset and cumulative incidence through midlife (p = 0.63). Heart failure differences are modest and emerge later, around age 60.
The gap opens around age 35
When does the divergence between men and women actually begin? This plot shows the gender difference by age:
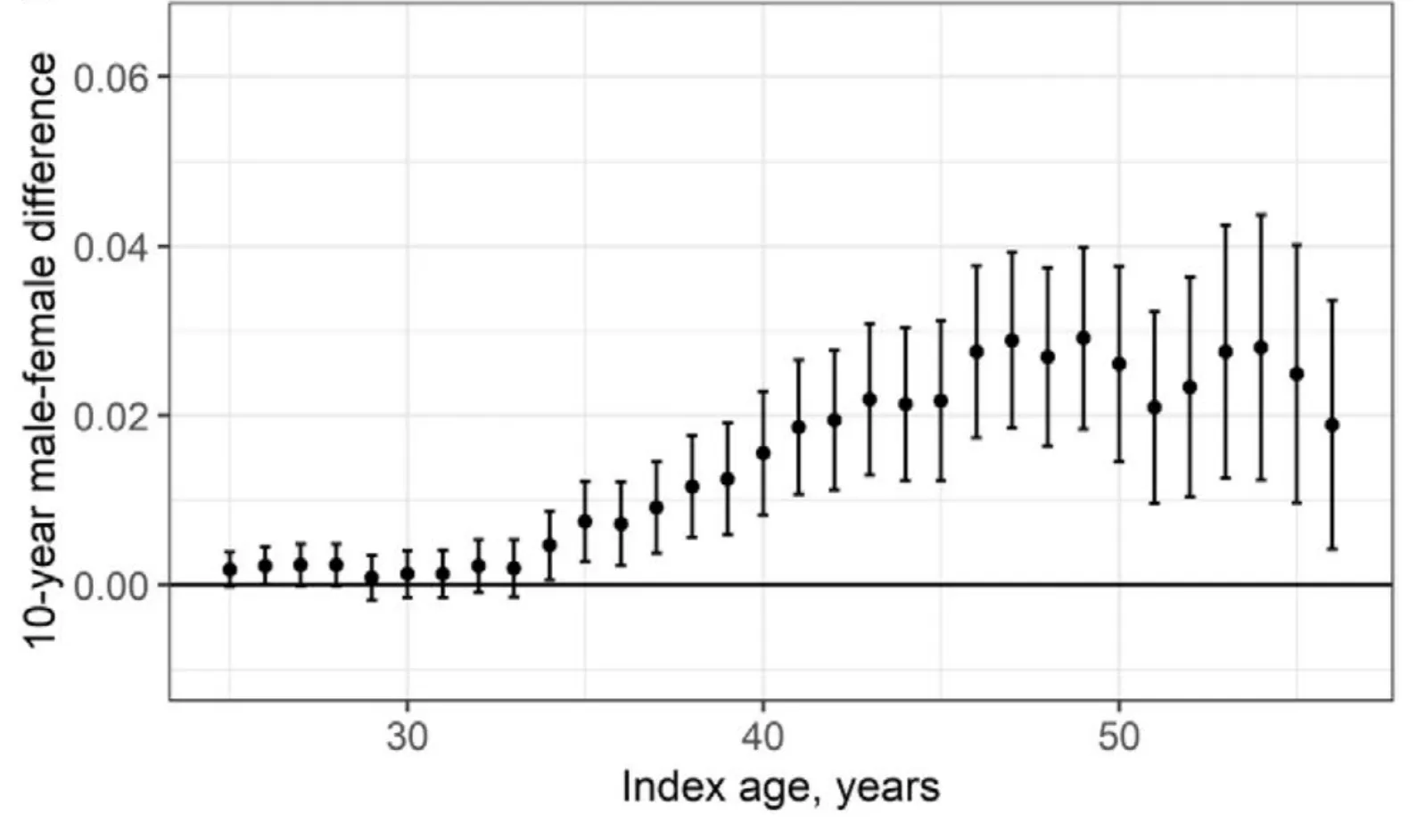 The 10-year difference in CVD risk between men and women, by age. The gap begins around age 35 and grows through midlife.
The 10-year difference in CVD risk between men and women, by age. The gap begins around age 35 and grows through midlife.
The gap is essentially zero through the late 20s. Around age 35, it begins to separate—and continues to widen through the 40s and 50s. By the late 40s, the excess 10-year risk for men is roughly 2–3 percentage points higher than for women.
If you’re a man in your mid-30s, your cardiovascular risk is already starting to diverge from a woman of the same age. The clock is ticking earlier than most people realize.
Traditional risk factors don’t fully explain the gap
The study adjusted for all seven components of the American Heart Association’s cardiovascular health framework: blood pressure, cholesterol, blood glucose, BMI, smoking, diet, and physical activity. These adjustments reduced the sex difference somewhat, but did not come close to eliminating it. Even when men and women have identical risk factor profiles, men still develop CVD earlier. The gap isn’t just about men smoking more or having worse diets. Something else is going on, likely a combination of hormonal, genetic, and vascular factors that we don’t yet fully understand.
How to test for cardiovascular disease
The study authors advocate for starting screening earlier, especially for men:
Cardiovascular disease risk differences emerging in the fourth decade of life supports initiating cardiovascular risk assessment and risk reduction strategies in young adulthood.
 Given a set of cardiovascular biomarkers, you can project heart disease risk across your lifetime and choose interventions to lower it.
Given a set of cardiovascular biomarkers, you can project heart disease risk across your lifetime and choose interventions to lower it.
There are six main biomarkers for heart disease:
-
ApoB measures the actual number of atherogenic particles in your blood. Think of ApoB as a more accurate cholesterol test. About 20% of people with normal LDL cholesterol have elevated ApoB.
-
Lp(a) is the strongest hereditary risk factor for heart disease. It’s genetically determined, doesn’t change much over your lifetime, and only needs to be measured once. If it’s elevated, you and your doctor can take a more aggressive approach to managing other risk factors.
-
hs-CRP measures systemic inflammation, which is increasingly recognized as an independent driver of cardiovascular events. The American College of Cardiology now recommends measuring it as part of cardiovascular risk assessment.
-
HbA1c captures your average blood sugar over 3 months and reflects metabolic health—another major contributor to cardiovascular risk.
-
eGFR measures kidney function (the amount of fluid your kidneys can filter). This is an input into the most recent risk equations.
-
Blood pressure is the strongest. While the latest wearables to have hypertension screening, the gold standard is a blood pressure cuff.
What this means
Heart disease hits men earlier than women, and the gap starts widening in the mid-30s. Traditional medical practice has only started risk assessment after age 40, but this study shows why being more proactive is a good idea. Given that one of the authors, Donald Lloyd-Jones, is behind the American Heart Association’s cardiovascular risk models, there’s real weight behind changing medical practice to be more proactive.
For men, I think te message is: don’t wait until 50 to take heart health seriously. The plaque that causes a heart attack at 55 doesn’t appear overnight. It builds over decades, starting in young adulthood. Getting a comprehensive set of cardiovascular biomarkers in your 30s gives you a baseline and a chance to intervene early.
For women, the gap doesn’t mean lower risk—just later onset. Women’s cardiovascular risk climbs steeply after menopause, and the same biomarkers and interventions can help you get ahead of the problem.
Get your free 30-day heart health guide
Evidence-based steps to optimize your heart health.
